Treatment Abroad – Find Verified Clinics, Reviews & Prices
Treatment Abroad made simple by A-Medical. Explore top clinics worldwide and start your journey toward better health today
We make healthcare abroad
simple, transparent, and fully guided from start to finish
Submit Your Request
Tell us about your treatment needs. We carefully review your case and match you with the most suitable hospitals and doctors.
Get Official Price Quotes
We provide verified treatment offers and proformas directly from hospitals — no middlemen, full transparency.
Connect with Doctors
We arrange direct calls or video consultations with hospitals and doctors so you can discuss your treatment plan confidently.
Confirm & Start Treatment
Once you accept the treatment plan, we schedule your hospital appointment and support you throughout your medical journey.
Clinics
Discover our network of world-class medical facilities offering comprehensive healthcare services
Why Choose Us
With us, you are in safe hands. We focus on quality, transparency, and patient-first care. Here’s what sets us apart
Only Accredited Hospitals
We partner exclusively with internationally accredited and top-ranked hospitals.
Direct & Transparent Payments
You pay directly at the hospital, with no hidden fees.
Free Direct Call & Video Consultation
Speak with our experts and doctors before making any decisions.
Best Doctor & Hospital Match
We carefully select the most suitable specialist and clinic for your treatment needs.
Worldwide Hospital Network
Access to a vast global network across 90+ countries.
More Affordable Pricing
We negotiate better prices from hospitals than you would get by contacting them directly.
Medical Conditions
Explore our comprehensive coverage of medical conditions and find the right treatment options
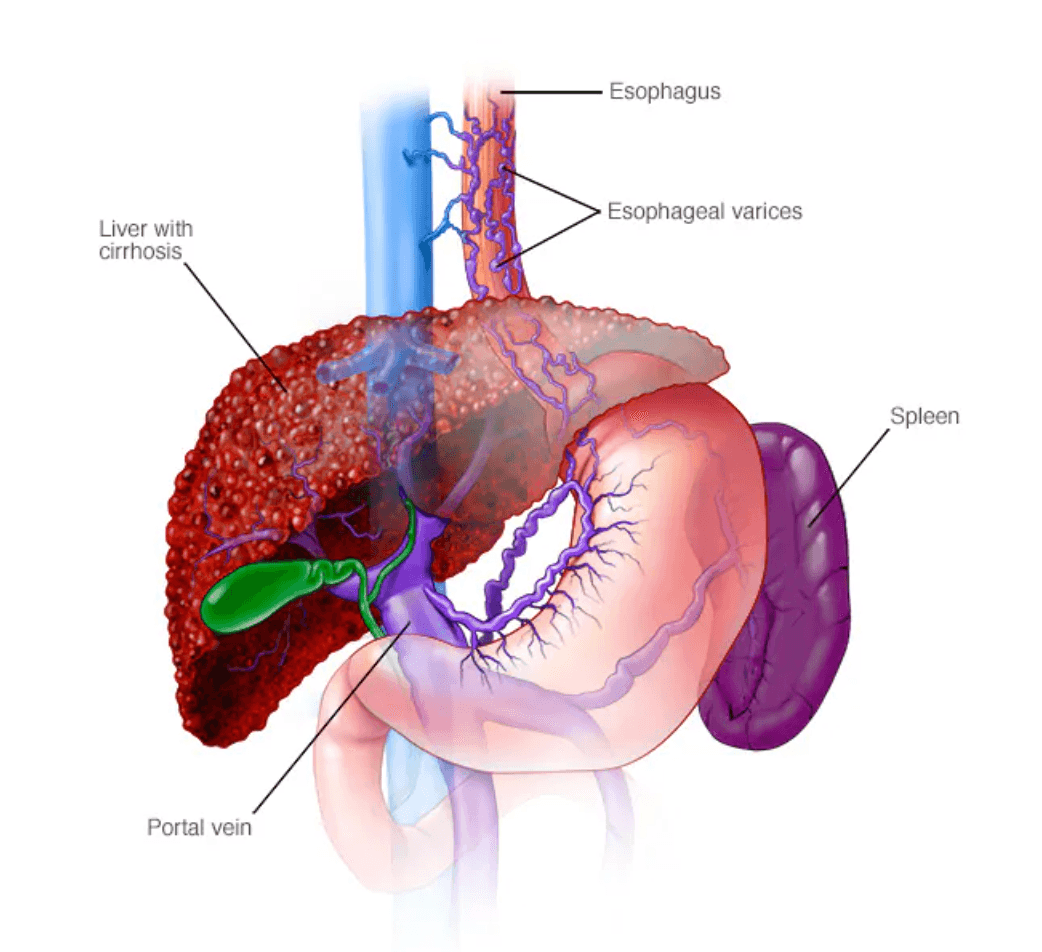
Esophageal varices
Esophageal varices are abnormally enlarged veins in the esophagus (the tube connecting the throat and stomach). They most often develop in people with advanced liver disease, especially cirrhosis. Why esophageal varices form When liver scarring blocks normal blood flow, pressure builds in the portal vein (portal hypertension). Blood is forced into smaller veins—such as those in the lower esophagus—that aren’t built to handle high pressure. These veins enlarge, can leak, and may rupture, causing life-threatening bleeding. Symptoms Varices usually don’t cause symptoms unless they bleed. Signs of bleeding include: Vomiting blood Black, tarry or bloody stools Lightheadedness or fainting from blood loss Loss of consciousness in severe cases People with liver disease may also have: Jaundice (yellow skin/eyes) Easy bruising or bleeding Ascites (fluid buildup in the abdomen) Emergency: Bloody vomit or black/bloody stools require immediate medical care (call 911). Causes Cirrhosis from hepatitis, alcohol-related liver disease, fatty liver disease, or primary biliary cholangitis Blood clots in the portal or splenic vein Schistosomiasis (parasitic infection in certain regions) Risk factors for bleeding High portal vein pressure Large varices Red streaks or spots seen on endoscopy Severe cirrhosis or liver failure Continued alcohol use Previous variceal bleeding Complications Massive bleeding, shock, and death High risk of recurrent bleeding after a first episode Prevention & management Varices themselves can’t always be prevented, but bleeding risk can be reduced: Nonselective beta blockers (e.g., propranolol, nadolol) to lower portal pressure Endoscopic screening for people with cirrhosis; band ligation for high-risk varices Avoid alcohol Healthy diet and weight management Protect the liver: safe sex, avoid needle sharing, get vaccinated for hepatitis A and B Use chemicals and medicines carefully If you have liver disease, ask your healthcare professional about screening and preventive treatment for esophageal varices.
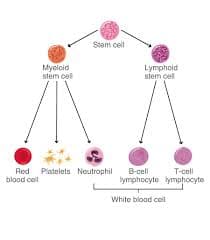
Chronic Lymphocytic Leukemia (CLL)
What Is Chronic Lymphocytic Leukemia (CLL)? Chronic lymphocytic leukemia (CLL) is a type of blood cancer that affects the bone marrow and blood. In a healthy body, blood stem cells mature into red blood cells, platelets, and white blood cells (lymphocytes) that help fight infection. In CLL, too many blood stem cells develop into abnormal lymphocytes, also called leukemia cells. These cells do not function properly and cannot fight infections effectively. As they accumulate in the bone marrow and bloodstream, they crowd out healthy blood cells. This can lead to anemia, increased risk of infections, and easy bruising or bleeding. CLL is considered a chronic leukemia, meaning it usually progresses slowly over time. Risk Factors for CLL The main risk factors associated with CLL include: Family history of CLL Family history of cancers of the lymphatic system Age over 70 Male sex White ethnicity Exposure to Agent Orange CLL does not appear to be linked to diet, infections, or smoking. Symptoms of CLL CLL often develops silently. Many people have the disease for years without symptoms and are diagnosed incidentally during routine blood tests for unrelated conditions. When symptoms do appear, they may include: Fatigue and weakness Enlarged lymph nodes (felt as painless lumps under the skin) Abdominal discomfort or a feeling of fullness due to an enlarged spleen Unexplained weight loss Night sweats Frequent or severe infections Types of CLL There are two main biological forms of CLL: Slow-growing (indolent) CLL, which may not require treatment for many years Faster-growing (aggressive) CLL, which progresses more rapidly and requires earlier treatment The difference between these types cannot be determined by symptoms alone. Specialized laboratory and genetic testing are required to identify the form of CLL and guide treatment decisions.
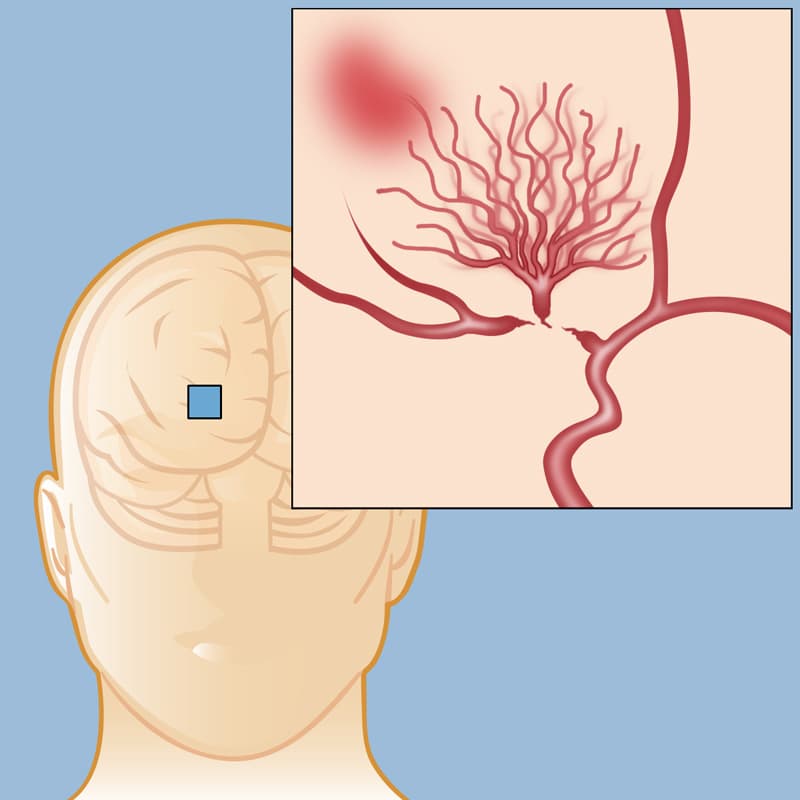
Moyamoya Disease
What Is Moyamoya Disease? Moyamoya disease is a rare, progressive cerebrovascular disorder in which the main arteries supplying blood to the brain—particularly the internal carotid arteries—become narrowed or blocked. As blood flow decreases, the brain compensates by forming a network of small, fragile blood vessels at its base to maintain circulation. These abnormal collateral vessels are prone to bleeding and clotting, significantly increasing the risk of recurrent strokes and transient ischaemic attacks (TIAs). The term “moyamoya”, meaning “puff of smoke” in Japanese, refers to the characteristic appearance of these tangled vessels seen on cerebral angiography. Although moyamoya disease is more commonly diagnosed in children, it can also affect adults, often presenting with different symptoms and complications. Types of Moyamoya Disease Idiopathic Moyamoya Disease This is the primary form, with no identifiable underlying cause. Secondary Moyamoya Syndrome This form develops in association with other medical conditions, including: Neurofibromatosis Down syndrome Previous radiation therapy to the head Certain genetic or systemic disorders Symptoms of Moyamoya Disease Symptoms vary depending on the patient’s age and the severity of arterial narrowing. Common signs and symptoms include: Sudden weakness or paralysis, often affecting one side of the body Recurrent transient ischaemic attacks (TIAs) or strokes Severe or persistent headaches Seizures (more common in children) Cognitive impairment, including memory and learning difficulties Visual disturbances or sudden vision loss Speech problems, such as difficulty speaking or understanding language Involuntary movements, including chorea or dystonia When to Seek Emergency Medical Care Immediate medical attention is critical if stroke symptoms are suspected. Remember FAST: F – Face: Facial drooping when smiling A – Arms: Weakness when raising one or both arms S – Speech: Slurred speech or difficulty understanding T – Time: Call emergency services immediately Prompt treatment can be life-saving and reduce long-term disability. Causes of Moyamoya Disease The exact cause of moyamoya disease remains unknown, but several contributing factors have been identified: Genetic predisposition: The condition may run in families and is more common among individuals of East Asian descent Autoimmune conditions: Diseases such as lupus may be associated Environmental factors: Previous radiation therapy to the brain increases risk Complications and Related Conditions Progressive narrowing of cerebral blood vessels can lead to serious neurological complications, including: Recurrent TIAs Ischaemic stroke (cerebral infarction) Haemorrhagic stroke Developmental delays and learning difficulties in children Permanent weakness or paralysis Speech and language disorders Seizure disorders Emotional and behavioural changes, including anxiety, depression, and personality changes Can Moyamoya Disease Be Prevented? Currently, there is no known method to prevent moyamoya disease, as its underlying cause is not fully understood. However, proactive management can reduce complications: Regular neurological evaluations for early diagnosis Genetic counselling for families with a known history Maintaining vascular health through: Balanced nutrition Regular physical activity Avoidance of smoking Early detection and appropriate medical or surgical management are key to improving long-term outcomes.
Get a free consultation
Talk to our experts and discover the best solution for your needs completely free of charge.

Related Articles
Stay informed with our latest medical insights and health tips

Top Clinics Worldwide for Stem Cell Therapy in Autism Treatment
his article explores the intricacies of stem cell therapy for autism, its benefits, costs, and top global clinics offering the treatment.

Burun Tutulması Səbəbləri və Müalicəsi
Burun tutulması, burun boşluqlarında hava axınının qismən və ya tam şəkildə məhdudlaşmasıdır.

Autism Treatment in Turkey - Best Clinics, Doctors and Costs
Autism treatment in Turkey offers affordable, high-quality care with fast access to therapy and experienced multidisciplinary teams. Families benefit from individualized programs, English-speaking spe...
Our doctor is highly skilled and an expert in their field.