Treatment Abroad – Find Verified Clinics, Reviews & Prices
Treatment Abroad made simple by A-Medical. Explore top clinics worldwide and start your journey toward better health today
We make healthcare abroad
simple, transparent, and fully guided from start to finish
Submit Your Request
Tell us about your treatment needs. We carefully review your case and match you with the most suitable hospitals and doctors.
Get Official Price Quotes
We provide verified treatment offers and proformas directly from hospitals — no middlemen, full transparency.
Connect with Doctors
We arrange direct calls or video consultations with hospitals and doctors so you can discuss your treatment plan confidently.
Confirm & Start Treatment
Once you accept the treatment plan, we schedule your hospital appointment and support you throughout your medical journey.
Clinics
Discover our network of world-class medical facilities offering comprehensive healthcare services
Why Choose Us
With us, you are in safe hands. We focus on quality, transparency, and patient-first care. Here’s what sets us apart
Only Accredited Hospitals
We partner exclusively with internationally accredited and top-ranked hospitals.
Direct & Transparent Payments
You pay directly at the hospital, with no hidden fees.
Free Direct Call & Video Consultation
Speak with our experts and doctors before making any decisions.
Best Doctor & Hospital Match
We carefully select the most suitable specialist and clinic for your treatment needs.
Worldwide Hospital Network
Access to a vast global network across 90+ countries.
More Affordable Pricing
We negotiate better prices from hospitals than you would get by contacting them directly.
Medical Conditions
Explore our comprehensive coverage of medical conditions and find the right treatment options

Stroke
Stroke
Hodgkin lymphoma (Hodgkin disease)
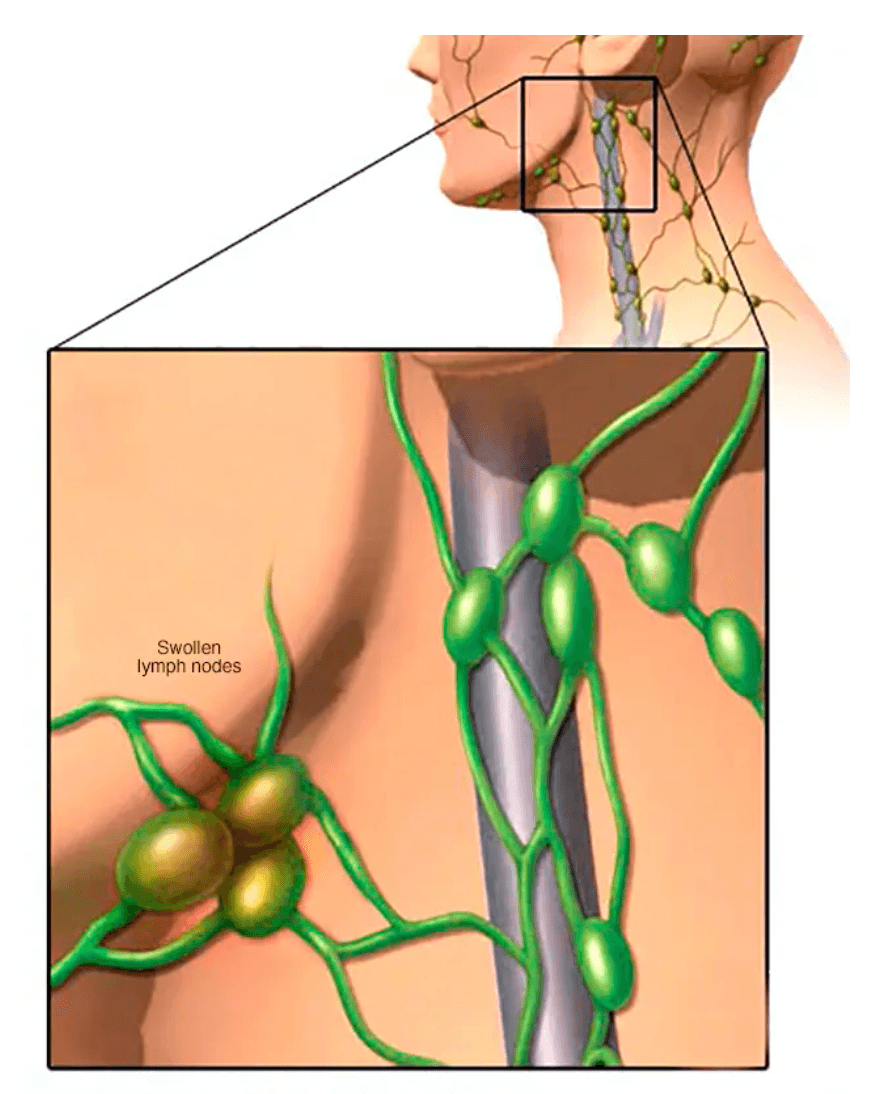
Hodgkin lymphoma is a type of lymphoma, a cancer that affects the lymphatic system—part of the body’s immune defense. The lymphatic system includes lymph nodes, lymph vessels, the spleen, thymus, tonsils, adenoids and bone marrow. Hodgkin lymphoma (formerly called Hodgkin disease) can involve any of these areas and sometimes other organs. Lymphomas are broadly divided into Hodgkin lymphoma and non-Hodgkin lymphoma. Hodgkin lymphoma begins in B lymphocytes, which are germ-fighting white blood cells. It is highly treatable and often curable, especially when diagnosed early. Types of Hodgkin Lymphoma 1. Classic Hodgkin Lymphoma This is the most common type. It is defined by the presence of Reed–Sternberg cells in affected lymph nodes. Subtypes include: Nodular sclerosing Hodgkin lymphoma Mixed cellularity Hodgkin lymphoma Lymphocyte-depleted classic Hodgkin lymphoma Lymphocyte-rich classic Hodgkin lymphoma 2. Nodular Lymphocyte-Predominant Hodgkin Lymphoma (NLPHL) A rarer form, characterized by so-called “popcorn cells.” It is often diagnosed at an early stage and may require less intensive treatment than classic Hodgkin lymphoma. Signs and Symptoms Common symptoms include: Swollen lymph nodes (neck, armpits or groin), usually painless Fever Persistent fatigue Drenching night sweats Unexplained weight loss Itchy skin When to See a Doctor Make an appointment with a healthcare professional if you notice persistent swollen lymph nodes or other symptoms that concern you. Early evaluation is important, as timely diagnosis greatly improves outcomes. Treatment Options Treatment depends on the type and stage of the disease and may include: Chemotherapy Radiation therapy Targeted therapy Immunotherapy Bone marrow (stem cell) transplant Clinical trials
Chronic Lymphocytic Leukemia (CLL)
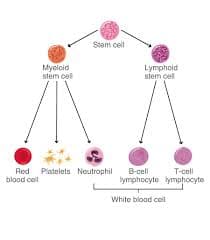
What Is Chronic Lymphocytic Leukemia (CLL)? Chronic lymphocytic leukemia (CLL) is a type of blood cancer that affects the bone marrow and blood. In a healthy body, blood stem cells mature into red blood cells, platelets, and white blood cells (lymphocytes) that help fight infection. In CLL, too many blood stem cells develop into abnormal lymphocytes, also called leukemia cells. These cells do not function properly and cannot fight infections effectively. As they accumulate in the bone marrow and bloodstream, they crowd out healthy blood cells. This can lead to anemia, increased risk of infections, and easy bruising or bleeding. CLL is considered a chronic leukemia, meaning it usually progresses slowly over time. Risk Factors for CLL The main risk factors associated with CLL include: Family history of CLL Family history of cancers of the lymphatic system Age over 70 Male sex White ethnicity Exposure to Agent Orange CLL does not appear to be linked to diet, infections, or smoking. Symptoms of CLL CLL often develops silently. Many people have the disease for years without symptoms and are diagnosed incidentally during routine blood tests for unrelated conditions. When symptoms do appear, they may include: Fatigue and weakness Enlarged lymph nodes (felt as painless lumps under the skin) Abdominal discomfort or a feeling of fullness due to an enlarged spleen Unexplained weight loss Night sweats Frequent or severe infections Types of CLL There are two main biological forms of CLL: Slow-growing (indolent) CLL, which may not require treatment for many years Faster-growing (aggressive) CLL, which progresses more rapidly and requires earlier treatment The difference between these types cannot be determined by symptoms alone. Specialized laboratory and genetic testing are required to identify the form of CLL and guide treatment decisions.
Get a free consultation
Talk to our experts and discover the best solution for your needs completely free of charge.

Related Articles
Stay informed with our latest medical insights and health tips

Retinal Transplant in Turkey - Best Clinics and Surgeons
People from around the world choose Turkey for retina transplant surgery. Highly skilled doctors in modern clinics, equipped with the latest medical technologies, perform these surgeries.

Best Countries for Panic Attack and Anxiety Treatment
Choosing the best country for panic attack treatment can be daunting, especially when considering options in foreign countries. A-Medical specializes in taking the stress out of this process by offeri...

Colon Cancer Treatment in Turkey - Best Clinics & Doctors
International patients highly prefer Turkey for colon treatment due to its cost-effectiveness and excellent medical services.
Our doctor is highly skilled and an expert in their field.









