Treatment Abroad – Find Verified Clinics, Reviews & Prices
Treatment Abroad made simple by A-Medical. Explore top clinics worldwide and start your journey toward better health today
We make healthcare abroad
simple, transparent, and fully guided from start to finish
Submit Your Request
Tell us about your treatment needs. We carefully review your case and match you with the most suitable hospitals and doctors.
Get Official Price Quotes
We provide verified treatment offers and proformas directly from hospitals — no middlemen, full transparency.
Connect with Doctors
We arrange direct calls or video consultations with hospitals and doctors so you can discuss your treatment plan confidently.
Confirm & Start Treatment
Once you accept the treatment plan, we schedule your hospital appointment and support you throughout your medical journey.
Clinics
Discover our network of world-class medical facilities offering comprehensive healthcare services
Why Choose Us
With us, you are in safe hands. We focus on quality, transparency, and patient-first care. Here’s what sets us apart
Only Accredited Hospitals
We partner exclusively with internationally accredited and top-ranked hospitals.
Direct & Transparent Payments
You pay directly at the hospital, with no hidden fees.
Free Direct Call & Video Consultation
Speak with our experts and doctors before making any decisions.
Best Doctor & Hospital Match
We carefully select the most suitable specialist and clinic for your treatment needs.
Worldwide Hospital Network
Access to a vast global network across 90+ countries.
More Affordable Pricing
We negotiate better prices from hospitals than you would get by contacting them directly.
Medical Conditions
Explore our comprehensive coverage of medical conditions and find the right treatment options
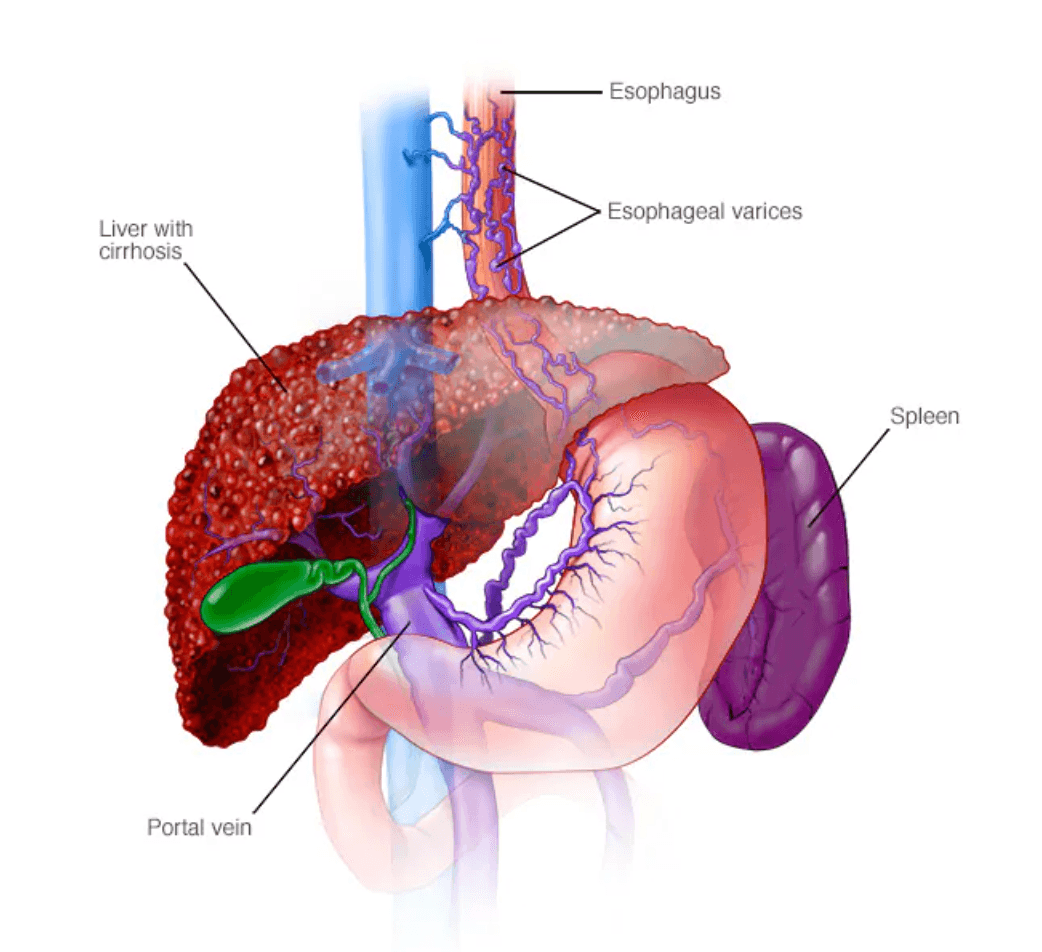
Esophageal varices
Esophageal varices are abnormally enlarged veins in the esophagus (the tube connecting the throat and stomach). They most often develop in people with advanced liver disease, especially cirrhosis. Why esophageal varices form When liver scarring blocks normal blood flow, pressure builds in the portal vein (portal hypertension). Blood is forced into smaller veins—such as those in the lower esophagus—that aren’t built to handle high pressure. These veins enlarge, can leak, and may rupture, causing life-threatening bleeding. Symptoms Varices usually don’t cause symptoms unless they bleed. Signs of bleeding include: Vomiting blood Black, tarry or bloody stools Lightheadedness or fainting from blood loss Loss of consciousness in severe cases People with liver disease may also have: Jaundice (yellow skin/eyes) Easy bruising or bleeding Ascites (fluid buildup in the abdomen) Emergency: Bloody vomit or black/bloody stools require immediate medical care (call 911). Causes Cirrhosis from hepatitis, alcohol-related liver disease, fatty liver disease, or primary biliary cholangitis Blood clots in the portal or splenic vein Schistosomiasis (parasitic infection in certain regions) Risk factors for bleeding High portal vein pressure Large varices Red streaks or spots seen on endoscopy Severe cirrhosis or liver failure Continued alcohol use Previous variceal bleeding Complications Massive bleeding, shock, and death High risk of recurrent bleeding after a first episode Prevention & management Varices themselves can’t always be prevented, but bleeding risk can be reduced: Nonselective beta blockers (e.g., propranolol, nadolol) to lower portal pressure Endoscopic screening for people with cirrhosis; band ligation for high-risk varices Avoid alcohol Healthy diet and weight management Protect the liver: safe sex, avoid needle sharing, get vaccinated for hepatitis A and B Use chemicals and medicines carefully If you have liver disease, ask your healthcare professional about screening and preventive treatment for esophageal varices.
Gaucher disease
Gaucher disease (go-SHAY) is a rare inherited metabolic disorder in which a fatty substance called glucocerebroside builds up in the body’s cells. This buildup mainly affects the spleen, liver, and bones, leading to organ enlargement, bone disease, and blood problems. More than 90% of cases are Type 1, the non-neurological form. Gaucher disease is more common among people of Ashkenazi Jewish (Eastern and Central European Jewish) ancestry. Types of Gaucher Disease Type 1 (Non-neuropathic) – most common Symptoms vary widely and can appear in childhood, adolescence, or adulthood. Common features include: Enlarged spleen and liver Easy bruising or bleeding (low platelets) Abdominal pain or fullness Bone disease Bone pain Fragile bones and fractures Bone marrow problems causing anemia and fatigue Growth delays in children (short stature, delayed puberty) Lung involvement (less common), including breathing difficulties Type 2 (Acute neuropathic) – rare and severe Symptoms begin in infancy Rapid damage to the brain stem Affects breathing, swallowing, and muscle control Life expectancy is usually under 2 years Type 3 (Chronic neuropathic) Combines Type 1 symptoms with progressive neurological involvement Begins in childhood Symptoms may include: Abnormal eye movements Muscle spasms and seizures Loss of muscle control Dementia in adolescence or early adulthood Causes Gaucher disease is caused by a mutation in the gene responsible for producing an enzyme that breaks down glucocerebroside. Without enough of this enzyme, the fatty substance accumulates inside white blood cells (called Gaucher cells), which then damage tissues and organs. Inheritance Autosomal recessive A child must inherit two mutated genes (one from each parent) to develop the disease People with only one mutated gene are carriers and usually have no symptoms Risk Factors Ashkenazi Jewish ancestry (especially for Type 1) Family history of Gaucher disease Complications (mainly Type 1) Increased risk of Parkinson’s disease and Lewy body dementia Higher risk of blood and bone marrow cancers Worsening symptoms during pregnancy Increased risk of bleeding after childbirth Treatment & Monitoring There is no cure, but effective treatments are available: Enzyme replacement therapy (ERT) to break down the fatty substance Substrate reduction therapy (SRT) to limit its production Regular monitoring to assess organ size, bone health, and blood counts With early diagnosis and proper treatment, many people with Type 1 Gaucher disease can live full, active lives. If you or your child have symptoms suggestive of Gaucher disease, or if it runs in your family, genetic testing and specialist evaluation are recommended.
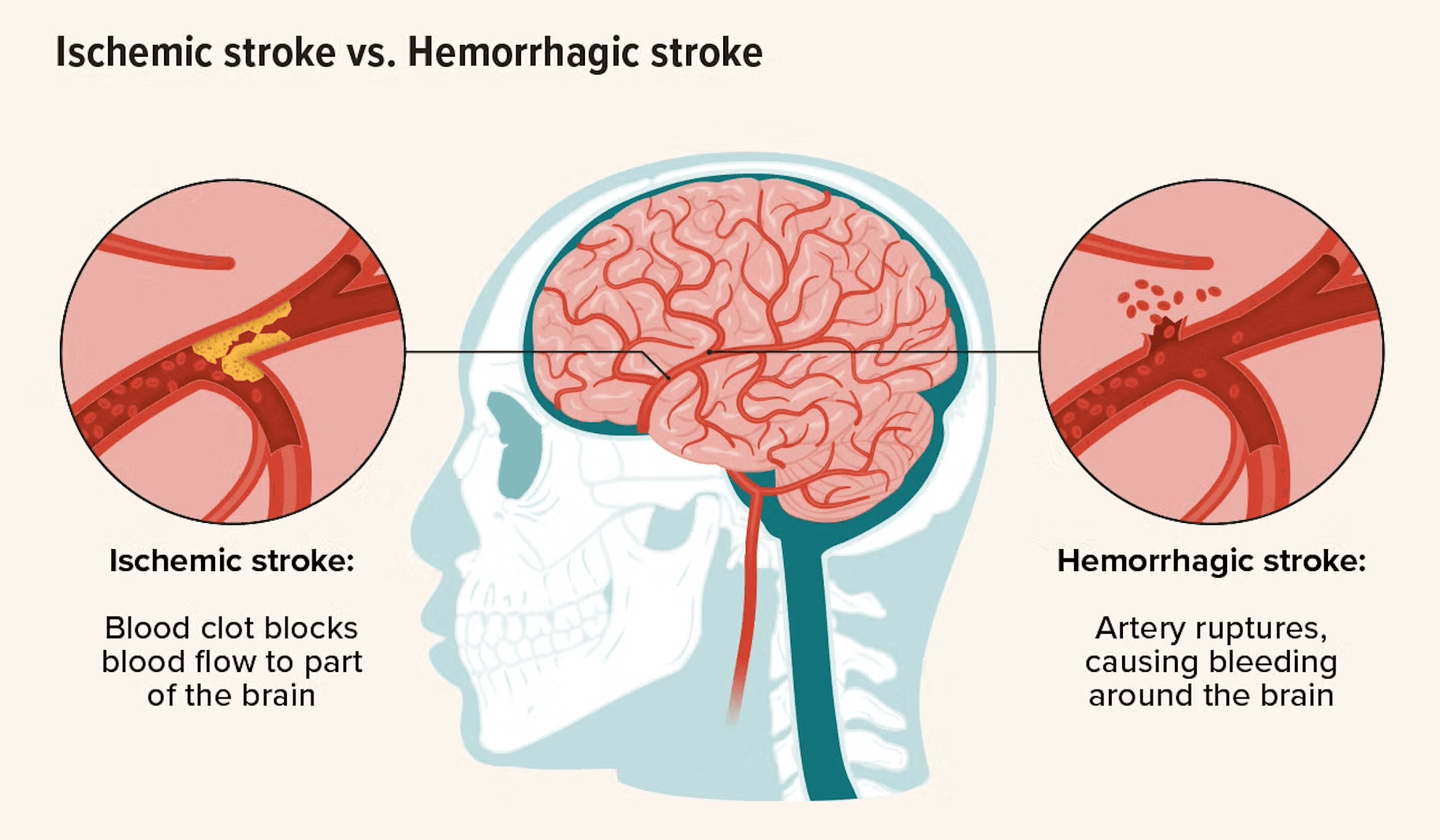
Ischaemic stroke
What is an ischaemic stroke? An ischaemic stroke, also called a cerebral infarction, happens when a blood clot or other obstruction blocks an artery supplying blood to the brain. This blockage sharply reduces blood flow, depriving brain tissue of oxygen and nutrients. Without oxygen, brain cells begin to die within minutes. Ischaemic strokes are the most common type of stroke, accounting for around 80% of all cases, and they are a medical emergency. Rapid treatment is critical to limit brain damage, disability, and life-threatening complications. Types of ischaemic stroke 1. Thrombotic stroke Caused by a blood clot (thrombus) that forms directly in an artery supplying the brain Commonly linked to atherosclerosis, where fatty plaques narrow the arteries Often develops during sleep or rest 2. Embolic stroke Occurs when a clot forms elsewhere in the body, most often in the heart The clot travels through the bloodstream and becomes lodged in a brain artery Frequently associated with atrial fibrillation, heart valve disease, or recent heart attack 3. Lacunar stroke Involves blockage of small, deep arteries within the brain Usually caused by long-standing high blood pressure leading to thickened vessel walls Can also be linked to diabetes or rare genetic conditions Symptoms of an ischaemic stroke Symptoms depend on which area of the brain is affected, but commonly include: Sudden numbness or weakness, especially on one side of the face, arm, or leg Sudden difficulty speaking or understanding speech Sudden vision problems in one or both eyes Sudden dizziness, loss of balance, or difficulty walking Sudden severe headache with no known cause When to seek emergency medical attention – ACT FAST Call emergency services immediately if you notice: F – Face drooping when smiling A – Arm weakness when raising one or both arms S – Speech difficulty or slurred speech T – Time to call emergency services Early treatment can be lifesaving and can significantly reduce long-term disability. What causes an ischaemic stroke? Several conditions can lead to artery blockage, including: Atherosclerosis (plaque build-up in arteries) Blood clots from the heart, often due to atrial fibrillation or heart valve disease High blood pressure, which damages and narrows blood vessels Carotid artery disease, causing reduced blood flow to the brain Blood disorders, such as sickle cell disease or clotting abnormalities Inflammatory or genetic blood vessel diseases Complications and related conditions An ischaemic stroke can cause long-term or permanent complications, such as: Paralysis or weakness, usually on one side of the body Speech and swallowing difficulties (dysphagia) Memory, concentration, and cognitive problems Chronic pain, numbness, or abnormal sensations Depression, anxiety, and emotional changes Secondary issues including pneumonia, pressure sores, or deep vein thrombosis due to reduced mobility How can ischaemic strokes be prevented? Prevention focuses on controlling risk factors and maintaining vascular health: Control blood pressure, diabetes, and cholesterol Eat a balanced, heart-healthy diet low in saturated fat and salt Exercise regularly Stop smoking and limit alcohol intake Take prescribed medications for heart rhythm disorders or clot prevention Attend regular health check-ups to monitor stroke risk factors
Get a free consultation
Talk to our experts and discover the best solution for your needs completely free of charge.

Related Articles
Stay informed with our latest medical insights and health tips
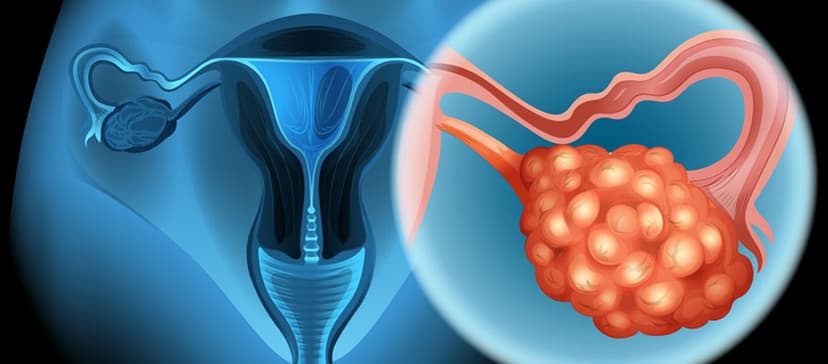
Gynecologic Oncology in Turkey - Best Clinics & Oncologists
This article explores gynecological oncology treatments in Turkey and highlights top Turkish specialists.

Best Schizophrenia Treatment Centers
Schizophrenia treatment abroad often becomes a real choice when patients feel that local options cannot give them the structure, time, or personal attention they need.

Cheapest Countries for Autism Treatment
Discover the cheapest countries for autism treatment with transparent pricing, reliable therapy programs, and experienced international clinics. Learn how Turkey, Georgia, Azerbaijan, Czechia, and Tha...
Our doctor is highly skilled and an expert in their field.









