Treatment Abroad – Find Verified Clinics, Reviews & Prices
Treatment Abroad made simple by A-Medical. Explore top clinics worldwide and start your journey toward better health today
We make healthcare abroad
simple, transparent, and fully guided from start to finish
Submit Your Request
Tell us about your treatment needs. We carefully review your case and match you with the most suitable hospitals and doctors.
Get Official Price Quotes
We provide verified treatment offers and proformas directly from hospitals — no middlemen, full transparency.
Connect with Doctors
We arrange direct calls or video consultations with hospitals and doctors so you can discuss your treatment plan confidently.
Confirm & Start Treatment
Once you accept the treatment plan, we schedule your hospital appointment and support you throughout your medical journey.
Clinics
Discover our network of world-class medical facilities offering comprehensive healthcare services
Why Choose Us
With us, you are in safe hands. We focus on quality, transparency, and patient-first care. Here’s what sets us apart
Only Accredited Hospitals
We partner exclusively with internationally accredited and top-ranked hospitals.
Direct & Transparent Payments
You pay directly at the hospital, with no hidden fees.
Free Direct Call & Video Consultation
Speak with our experts and doctors before making any decisions.
Best Doctor & Hospital Match
We carefully select the most suitable specialist and clinic for your treatment needs.
Worldwide Hospital Network
Access to a vast global network across 90+ countries.
More Affordable Pricing
We negotiate better prices from hospitals than you would get by contacting them directly.
Medical Conditions
Explore our comprehensive coverage of medical conditions and find the right treatment options
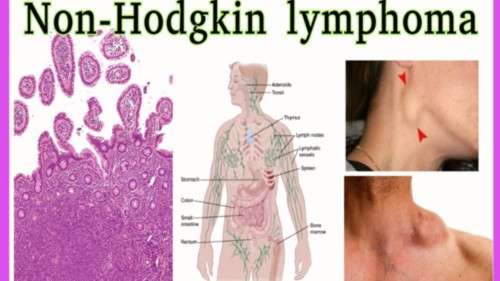
Non-Hodgkin lymphoma (NHL)
Non-Hodgkin lymphoma is a type of cancer that begins in the lymphatic system, which is part of the body’s immune system. The lymphatic system includes lymph nodes, lymph vessels, and organs such as the spleen, thymus, tonsils, adenoids, and bone marrow. It helps the body fight infections and other diseases. Non-Hodgkin lymphoma can develop in any part of the lymphatic system and may also spread to other organs in the body. There are many different forms of lymphoma, which are generally classified into two main groups: Hodgkin lymphoma and non-Hodgkin lymphoma. Non-Hodgkin lymphoma is the more common of the two. Most types of non-Hodgkin lymphoma begin in B lymphocytes (B cells) or T lymphocytes (T cells), which are white blood cells that play key roles in the immune response.
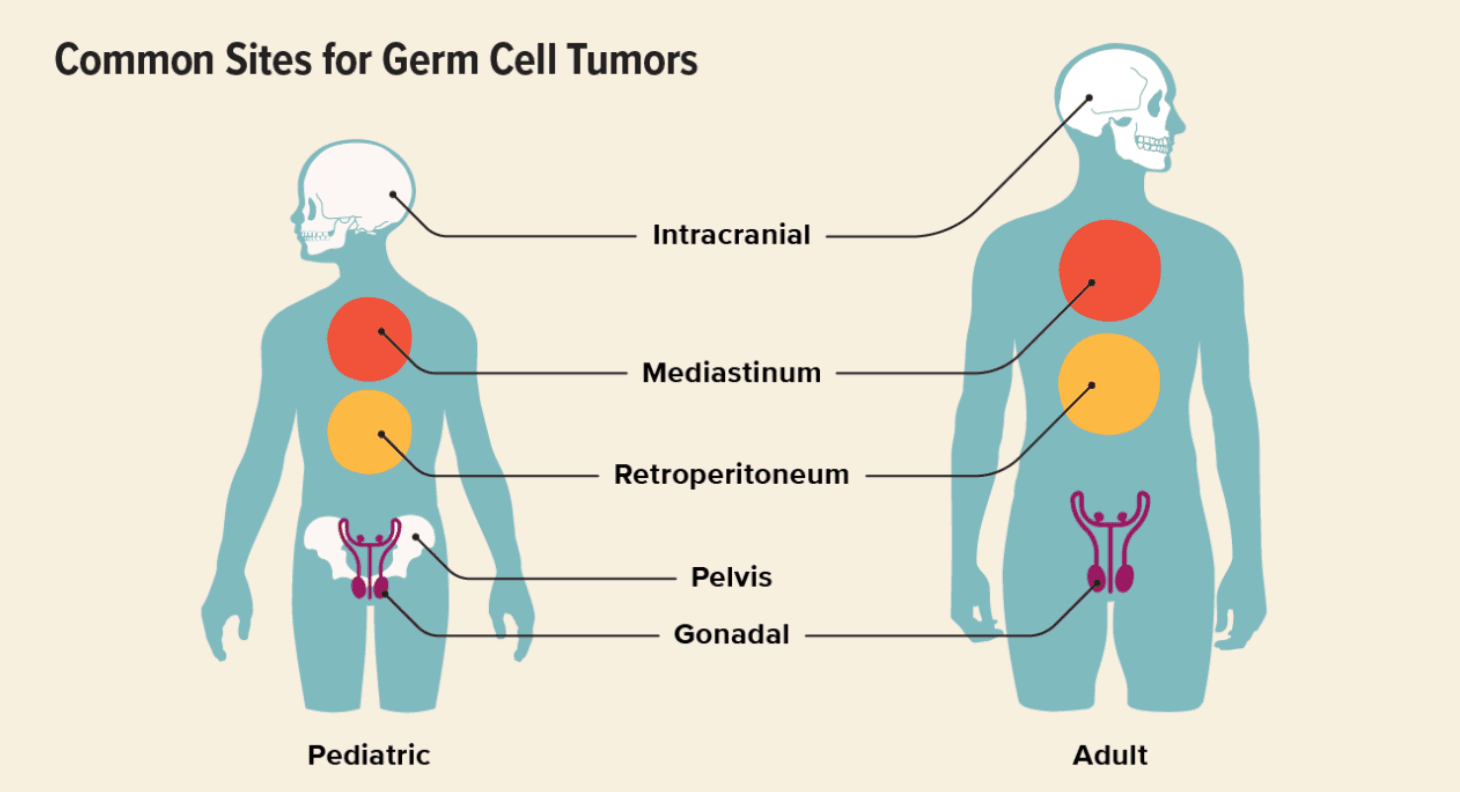
Germ Cell Tumor
Germ cells, also called gametes, are specialized cells responsible for sexual reproduction. Their name comes from the word germinate, meaning “to begin to grow.” During fetal development, germ cells migrate to specific locations and later develop into sperm in males or egg cells (ova) in females. In some cases, germ cells undergo abnormal growth and form a germ cell tumor (GCT). These tumors most commonly develop in the testicles or ovaries, but in rare cases, they can appear in other parts of the body. Germ cell tumors are rare and most often occur in adolescents and young adults between ages 15 and 30, though they can affect children and older adults as well. Types of Germ Cell Tumors Germ cell tumors can be classified by behavior, sex, and location. By Behavior Benign (non-cancerous) Malignant (cancerous) By Sex In males (testicular germ cell tumors): Seminoma Non-seminoma In females (ovarian germ cell tumors): Dysgerminoma Non-dysgerminoma Other Germ Cell Tumor Types Teratoma (benign or malignant) Choriocarcinoma Germinoma Embryonal carcinoma Endodermal sinus tumor (yolk sac tumor) Polyembryoma Mixed germ cell tumors Extragonadal Germ Cell Tumors In rare cases, germ cell tumors develop outside the ovaries or testicles. These are called extragonadal germ cell tumors and may appear in: Mediastinum (chest) Pineal region of the brain Retroperitoneum (back of the abdomen) Sacrococcygeal area (base of the spine) Causes and Risk Factors The exact cause of germ cell tumors is not fully understood, but several factors increase risk: Genetic syndromes (e.g., Turner syndrome, Klinefelter syndrome) Birth defects involving the genitals, spine, or urinary tract Cryptorchidism (undescended testicle) Age, especially males aged 15–35 and adolescent girls or young women Germ Cell Tumor Symptoms Symptoms depend on the tumor’s type and location. Ovarian Germ Cell Tumors Abdominal swelling Pelvic pain Constipation Irregular vaginal bleeding Testicular Germ Cell Tumors Testicular lump or swelling Groin pain Heaviness in the scrotum Extragonadal Germ Cell Tumors Breathing difficulty (mediastinal tumors) Urinary problems Leg weakness or neurological symptoms (spinal involvement) Diagnosis Early detection is critical. Diagnostic tests may include: Physical examination Imaging tests (ultrasound, CT scan, MRI) Blood tests (tumor markers such as AFP, β-hCG, LDH) Biopsy or surgical removal for definitive diagnosis Germ Cell Tumor Staging Staging determines how far the tumor has spread and guides treatment. Stage 1 Tumor confined to the original site Often treated with surgery alone Stage 2 Spread to nearby tissues or structures Still localized to the pelvic or regional area Stage 3 Spread to distant areas or regional lymph nodes Stage 4 Metastasis to distant organs Common sites: lungs, liver, distant lymph nodes Germ Cell Tumor Treatment Treatment is individualized based on tumor type, stage, and patient factors. Surgery First-line treatment for localized tumors May involve removal of the tumor and, if necessary, the affected ovary or testicle Fertility-sparing surgery is often possible Chemotherapy Highly effective because germ cell tumors are very chemo-sensitive Used for advanced, aggressive, or metastatic disease Radiotherapy may be added in select cases Immunotherapy Used in relapsed or chemotherapy-resistant tumors Helps the immune system target cancer cells Prognosis Germ cell tumors generally have an excellent prognosis, especially when diagnosed early. Testicular germ cell tumors: ~95% survival rate Ovarian germ cell tumors: ~93% survival rate Outcomes depend on tumor location, stage at diagnosis, response to treatment, and overall patient health.
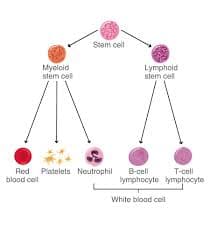
Chronic Myelogenous Leukemia (CML)
The bone marrow plays a critical role in the body’s ability to defend itself by producing blood cells. In healthy individuals, the bone marrow generates stem cells, which mature into: White blood cells (fight infection) Red blood cells (carry oxygen) Platelets (help blood clot) Leukemia develops when abnormalities occur in these stem cells, leading to uncontrolled production of abnormal white blood cells that circulate in the bloodstream and interfere with normal blood cell formation. What Is Chronic Myeloid Leukemia? Chronic myeloid leukemia (CML)—also called chronic granulocytic leukemia or chronic myelogenous leukemia—is a rare cancer of the bone marrow that primarily affects myeloid white blood cells. CML can occur at almost any age, but it is most commonly diagnosed in middle-aged and older adults. In CML, the bone marrow produces excessive numbers of immature myeloid cells, known as blasts, which crowd out healthy blood cells and disrupt normal blood function. Myeloid cells include: Granulocytes Monocytes Macrophages Dendritic cells When produced in abnormal quantities, these cells can lead to the development of CML. Phases of Chronic Myeloid Leukemia The term “chronic” refers to the disease’s typically slow progression. However, CML can advance into a more aggressive leukemia if not adequately controlled. CML is divided into three phases: 1. Chronic Phase Most patients are diagnosed during this phase Often discovered during routine blood tests Few or no symptoms Usually well controlled with medication 2. Accelerated Phase Increased number of immature blood cells Worsening symptoms Enlarged spleen Low red blood cell count Abnormal white blood cell levels May occur due to drug resistance 3. Blast Phase (Blast Crisis) Large numbers of immature blast cells Symptoms resemble acute leukemia High risk of infection, bleeding, and shortness of breath Can transform into acute myeloid leukemia (AML) Requires immediate medical treatment Relapsed CML Some patients may experience relapse, even after achieving remission. This can occur when leukemia cells develop resistance, often due to mutations in the BCR-ABL1 gene. Treatment for relapsed CML focuses on returning the disease to the chronic phase, most commonly using targeted therapy with tyrosine kinase inhibitors (TKIs). Causes of CML CML is caused by a genetic mutation in bone marrow stem cells. The hallmark of the disease is the Philadelphia chromosome. The Philadelphia Chromosome Results from a reciprocal translocation between chromosome 9 and chromosome 22 Produces an abnormal gene called BCR-ABL BCR-ABL creates a protein called tyrosine kinase This protein causes uncontrolled growth of abnormal white blood cells The Philadelphia chromosome develops after birth and is not inherited. Risk Factors for CML Risk factors increase the likelihood of developing cancer but do not guarantee it. Known risk factors include: Age: Average age at diagnosis is around 64 Radiation exposure: Seen in survivors of atomic bomb exposure and certain radiation-treated conditions Gender: More common in men Philadelphia chromosome: Present in nearly all CML cases CML is extremely rare in children and adolescents. Symptoms of CML CML can take years to develop and is often asymptomatic in early stages. When symptoms occur, they may include: Fatigue and weakness Shortness of breath during routine activity Pale or dull skin Fullness or discomfort in the left upper abdomen (enlarged spleen) Night sweats Fever Unintentional weight loss Bone pain Loss of appetite Easy bleeding or bruising Potential Complications Complications of CML may include: Anemia due to low red blood cell production Enlarged spleen Increased risk of secondary cancers, including thyroid, lung, stomach, prostate, and small bowel cancers Diagnosing Chronic Myeloid Leukemia Many patients are diagnosed incidentally after abnormal blood test results. Diagnosis involves specialized blood and bone marrow testing, analyzed by hematopathology experts. Diagnostic tests include: Complete blood count (CBC) with differential Peripheral blood smear Bone marrow aspiration and biopsy Cytogenetic analysis to detect the Philadelphia chromosome Fluorescence in situ hybridization (FISH) Quantitative polymerase chain reaction (qPCR) to measure BCR-ABL1 gene levels qPCR is the most sensitive test and is also used to monitor treatment response. Treatment Options for CML Treatment depends on disease phase, genetic findings, and overall health. Common treatment options include: Targeted therapy (Tyrosine Kinase Inhibitors) Blocks the BCR-ABL protein driving leukemia growth Chemotherapy Slows or stops leukemia cell division Radiation therapy Used in specific situations, such as spleen enlargement Bone marrow (stem cell) transplant Considered when drug therapy is unsuccessful CAR-T cell therapy Primarily used for other leukemias (e.g., ALL), but part of advanced immunotherapy programs Comprehensive Care and Quality of Life At Sheba, treatment extends beyond medication. Patients receive multidisciplinary support from: Hematologists and oncologists Nurses and transplant specialists Social workers and psychologists Nutritionists and supportive care teams The goal is not only to treat the disease but to preserve quality of life, emotional well-being, and long-term health. Living with Chronic Myeloid Leukemia CML is often a long-term condition. Even with a good prognosis, living with a chronic cancer can be emotionally challenging. Some patients require lifelong monitoring and treatment, which can complicate future planning. You do not have to face CML alone. With expert care, modern targeted therapies, and strong support systems, many people with CML lead long, productive, and fulfilling lives.
Get a free consultation
Talk to our experts and discover the best solution for your needs completely free of charge.

Related Articles
Stay informed with our latest medical insights and health tips

Melanoma (Skin Cancer) Treatment in Turkey - Best Clinics
Melanoma treatment in Turkey is a common procedure for addressing skin cancer, particularly when caused by abnormal melanocyte activity responsible for skin pigmentation.

8 Best and Cheapest Countries for Dentures 2025
The best and cheapest countries for veneers or best and cheapest countries for dental prostheses include Turkey, Thailand, and Mexico, where clinics offer modern technology, experienced specialists, a...
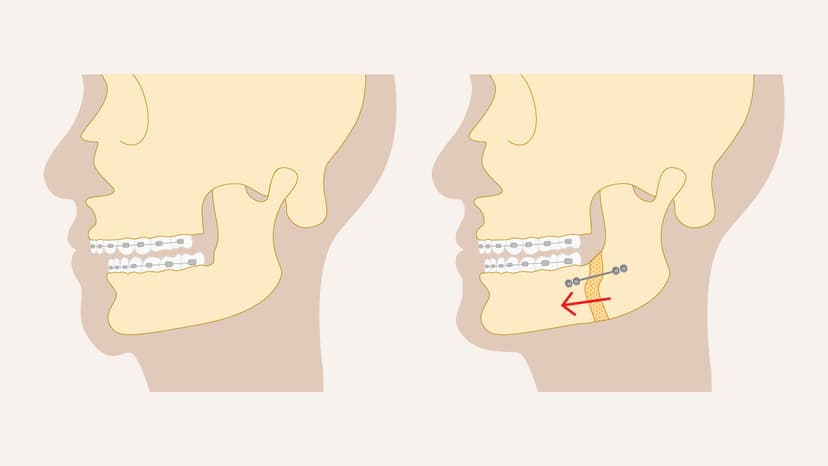
Orthognathic Surgery (Jaw Surgery) in Turkey
This guide provides essential details for those considering orthognathic surgery in Turkey. Discover top clinics, costs, and the procedure specifics here.
Our doctor is highly skilled and an expert in their field.









