Treatment Abroad – Find Verified Clinics, Reviews & Prices
Treatment Abroad made simple by A-Medical. Explore top clinics worldwide and start your journey toward better health today
We make healthcare abroad
simple, transparent, and fully guided from start to finish
Submit Your Request
Tell us about your treatment needs. We carefully review your case and match you with the most suitable hospitals and doctors.
Get Official Price Quotes
We provide verified treatment offers and proformas directly from hospitals — no middlemen, full transparency.
Connect with Doctors
We arrange direct calls or video consultations with hospitals and doctors so you can discuss your treatment plan confidently.
Confirm & Start Treatment
Once you accept the treatment plan, we schedule your hospital appointment and support you throughout your medical journey.
Clinics
Discover our network of world-class medical facilities offering comprehensive healthcare services
Why Choose Us
With us, you are in safe hands. We focus on quality, transparency, and patient-first care. Here’s what sets us apart
Only Accredited Hospitals
We partner exclusively with internationally accredited and top-ranked hospitals.
Direct & Transparent Payments
You pay directly at the hospital, with no hidden fees.
Free Direct Call & Video Consultation
Speak with our experts and doctors before making any decisions.
Best Doctor & Hospital Match
We carefully select the most suitable specialist and clinic for your treatment needs.
Worldwide Hospital Network
Access to a vast global network across 90+ countries.
More Affordable Pricing
We negotiate better prices from hospitals than you would get by contacting them directly.
Medical Conditions
Explore our comprehensive coverage of medical conditions and find the right treatment options

Prescription drug abuse
Prescription drug abuse—also called prescription drug misuse—means using a prescription medicine in a way not intended by the prescriber. This can range from taking someone else’s painkiller to crushing, snorting or injecting pills to get high. Misuse can become ongoing and compulsive despite harmful consequences. Prescription drug abuse affects all ages, including teens. The most commonly misused drugs are opioid painkillers, anti-anxiety medicines and sedatives, and stimulants. Early recognition and intervention can prevent misuse from progressing to addiction. Commonly misused prescription drugs Opioids (e.g., oxycodone, hydrocodone) Anti-anxiety medicines and sedatives (e.g., alprazolam, diazepam, zolpidem) Stimulants (e.g., methylphenidate, amphetamines) Signs and symptoms Opioids: constipation, nausea, drowsiness, slowed breathing, confusion, poor coordination, increased tolerance Sedatives: drowsiness, slurred speech, poor memory, unsteady walking, slowed breathing Stimulants: agitation, insomnia, high blood pressure, irregular heartbeat, anxiety, paranoia Other warning signs: taking higher doses than prescribed, early refill requests, “losing” prescriptions, mood swings, poor decisions, seeking prescriptions from multiple doctors. When to see a doctor If you’re concerned about your prescription drug use, talk to a healthcare professional early. They are trained to help, not judge. Causes and risk factors People may misuse prescription drugs to relieve pain or stress, improve performance, feel high, or avoid withdrawal. Risk factors include a personal or family history of addiction, mental health conditions, peer pressure, easy access to medications, and lack of awareness of risks. Older adults are also at risk, especially when mixing medicines with alcohol. Complications Prescription drug abuse can lead to overdose, coma or death; heart problems; seizures; addiction; accidents; legal trouble; and relationship or work problems. Prevention Take medicines only as prescribed and follow directions carefully. Check in regularly with your healthcare provider. Never use someone else’s prescription. Avoid mixing medicines with alcohol unless approved. Store medications securely and dispose of unused drugs properly. For teens: talk openly about risks, set clear rules, monitor medications at home, discourage online drug purchases, and stress the dangers of mixing drugs with alcohol.
Chronic Myelogenous Leukemia (CML)
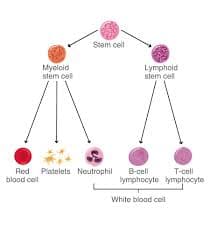
The bone marrow plays a critical role in the body’s ability to defend itself by producing blood cells. In healthy individuals, the bone marrow generates stem cells, which mature into: White blood cells (fight infection) Red blood cells (carry oxygen) Platelets (help blood clot) Leukemia develops when abnormalities occur in these stem cells, leading to uncontrolled production of abnormal white blood cells that circulate in the bloodstream and interfere with normal blood cell formation. What Is Chronic Myeloid Leukemia? Chronic myeloid leukemia (CML)—also called chronic granulocytic leukemia or chronic myelogenous leukemia—is a rare cancer of the bone marrow that primarily affects myeloid white blood cells. CML can occur at almost any age, but it is most commonly diagnosed in middle-aged and older adults. In CML, the bone marrow produces excessive numbers of immature myeloid cells, known as blasts, which crowd out healthy blood cells and disrupt normal blood function. Myeloid cells include: Granulocytes Monocytes Macrophages Dendritic cells When produced in abnormal quantities, these cells can lead to the development of CML. Phases of Chronic Myeloid Leukemia The term “chronic” refers to the disease’s typically slow progression. However, CML can advance into a more aggressive leukemia if not adequately controlled. CML is divided into three phases: 1. Chronic Phase Most patients are diagnosed during this phase Often discovered during routine blood tests Few or no symptoms Usually well controlled with medication 2. Accelerated Phase Increased number of immature blood cells Worsening symptoms Enlarged spleen Low red blood cell count Abnormal white blood cell levels May occur due to drug resistance 3. Blast Phase (Blast Crisis) Large numbers of immature blast cells Symptoms resemble acute leukemia High risk of infection, bleeding, and shortness of breath Can transform into acute myeloid leukemia (AML) Requires immediate medical treatment Relapsed CML Some patients may experience relapse, even after achieving remission. This can occur when leukemia cells develop resistance, often due to mutations in the BCR-ABL1 gene. Treatment for relapsed CML focuses on returning the disease to the chronic phase, most commonly using targeted therapy with tyrosine kinase inhibitors (TKIs). Causes of CML CML is caused by a genetic mutation in bone marrow stem cells. The hallmark of the disease is the Philadelphia chromosome. The Philadelphia Chromosome Results from a reciprocal translocation between chromosome 9 and chromosome 22 Produces an abnormal gene called BCR-ABL BCR-ABL creates a protein called tyrosine kinase This protein causes uncontrolled growth of abnormal white blood cells The Philadelphia chromosome develops after birth and is not inherited. Risk Factors for CML Risk factors increase the likelihood of developing cancer but do not guarantee it. Known risk factors include: Age: Average age at diagnosis is around 64 Radiation exposure: Seen in survivors of atomic bomb exposure and certain radiation-treated conditions Gender: More common in men Philadelphia chromosome: Present in nearly all CML cases CML is extremely rare in children and adolescents. Symptoms of CML CML can take years to develop and is often asymptomatic in early stages. When symptoms occur, they may include: Fatigue and weakness Shortness of breath during routine activity Pale or dull skin Fullness or discomfort in the left upper abdomen (enlarged spleen) Night sweats Fever Unintentional weight loss Bone pain Loss of appetite Easy bleeding or bruising Potential Complications Complications of CML may include: Anemia due to low red blood cell production Enlarged spleen Increased risk of secondary cancers, including thyroid, lung, stomach, prostate, and small bowel cancers Diagnosing Chronic Myeloid Leukemia Many patients are diagnosed incidentally after abnormal blood test results. Diagnosis involves specialized blood and bone marrow testing, analyzed by hematopathology experts. Diagnostic tests include: Complete blood count (CBC) with differential Peripheral blood smear Bone marrow aspiration and biopsy Cytogenetic analysis to detect the Philadelphia chromosome Fluorescence in situ hybridization (FISH) Quantitative polymerase chain reaction (qPCR) to measure BCR-ABL1 gene levels qPCR is the most sensitive test and is also used to monitor treatment response. Treatment Options for CML Treatment depends on disease phase, genetic findings, and overall health. Common treatment options include: Targeted therapy (Tyrosine Kinase Inhibitors) Blocks the BCR-ABL protein driving leukemia growth Chemotherapy Slows or stops leukemia cell division Radiation therapy Used in specific situations, such as spleen enlargement Bone marrow (stem cell) transplant Considered when drug therapy is unsuccessful CAR-T cell therapy Primarily used for other leukemias (e.g., ALL), but part of advanced immunotherapy programs Comprehensive Care and Quality of Life At Sheba, treatment extends beyond medication. Patients receive multidisciplinary support from: Hematologists and oncologists Nurses and transplant specialists Social workers and psychologists Nutritionists and supportive care teams The goal is not only to treat the disease but to preserve quality of life, emotional well-being, and long-term health. Living with Chronic Myeloid Leukemia CML is often a long-term condition. Even with a good prognosis, living with a chronic cancer can be emotionally challenging. Some patients require lifelong monitoring and treatment, which can complicate future planning. You do not have to face CML alone. With expert care, modern targeted therapies, and strong support systems, many people with CML lead long, productive, and fulfilling lives.
Myelofibrosis (MF)
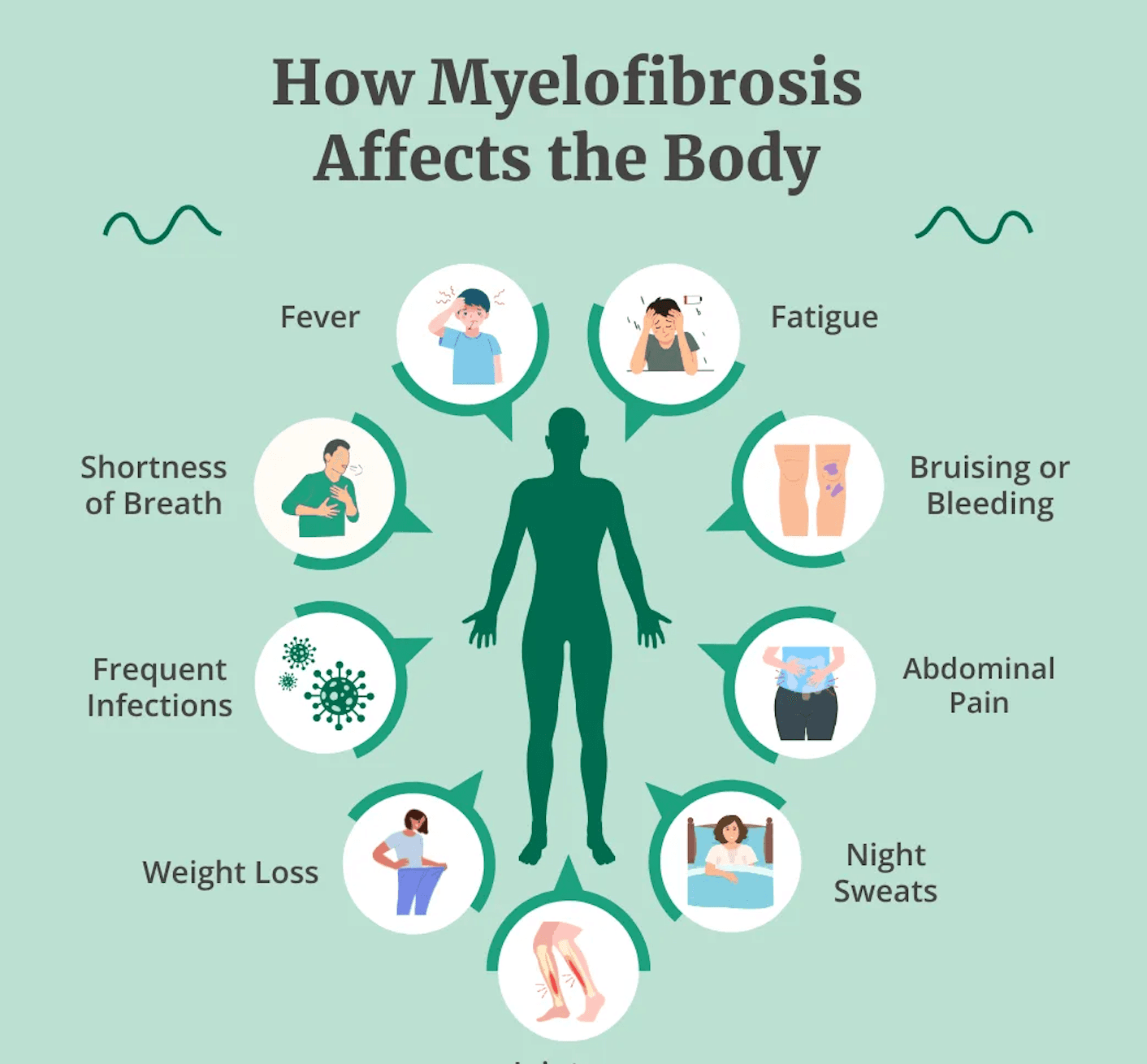
What Is Myelofibrosis? Myelofibrosis (MF) is a rare type of chronic blood cancer that originates in the bone marrow. In MF, healthy bone marrow tissue is gradually replaced by fibrous scar tissue, a process known as fibrosis. This scarring disrupts the bone marrow’s ability to produce normal blood cells, including red blood cells, white blood cells, and platelets. Myelofibrosis is usually a slow-growing disease, and many people live with it for years without noticeable symptoms. In some cases, however, MF progresses more rapidly and requires timely medical treatment. A hallmark feature of myelofibrosis is the overproduction of megakaryocytes — large bone marrow cells that normally produce platelets. In MF, these cells release excessive amounts of cytokines, proteins that promote inflammation. This chronic inflammation stimulates further scarring in the bone marrow, worsening blood cell production over time. Risk Factors for Myelofibrosis The exact cause of myelofibrosis is not fully understood. However, several factors are associated with an increased risk: Age: Most commonly diagnosed in people over 60 Environmental exposure: Ionizing radiation and petrochemicals such as benzene and toluene JAK2 mutation: Present in approximately 50–60% of MF patients; this mutation causes blood cells to grow and divide abnormally CALR mutation: Found in about 35% of people with MF Other genetic mutations may also play a role, although they are less common. Symptoms of Myelofibrosis Because MF often develops slowly, many patients experience no symptoms in the early stages. As the disease progresses and blood cell production becomes increasingly impaired, symptoms may include: Anemia, leading to fatigue, weakness, and shortness of breath Frequent infections Itching Pale skin Night sweats Fever Unexplained weight loss Abnormal bleeding or easy bruising Bone or joint pain Enlarged spleen (splenomegaly), causing discomfort or a feeling of fullness in the upper left abdomen Enlarged liver Dilated veins in the stomach or esophagus, which may rupture and bleed Portal hypertension, increased blood pressure in the vein connecting the spleen and liver Unexplained blood clots Extramedullary hematopoiesis, where blood-forming cells grow outside the bone marrow, potentially forming masses that compress organs or interfere with their function Types of Myelofibrosis Myelofibrosis is considered a rare form of chronic leukemia and is classified into two main types: Primary myelofibrosis: Occurs on its own, without a prior bone marrow disorder Secondary myelofibrosis: Develops as a complication of another bone marrow disease, such as polycythemia vera or essential thrombocythemia In approximately 12% of primary myelofibrosis cases, the disease can progress to acute myeloid leukemia (AML), a more aggressive and fast-growing cancer.
Get a free consultation
Talk to our experts and discover the best solution for your needs completely free of charge.

Related Articles
Stay informed with our latest medical insights and health tips

Stem Cell Therapy in Switzerland: Best Clinics & Doctors
Stem cell therapy in Switzerland offers safety, transparency, and clinical reliability. These are qualities that are non-negotiable for many patients seeking regenerative treatments.

7 Best and Cheapest Countries for All-on-6 Dental Implants Abroad
Are you considering an all-on-6 dental implant abroad but worried about cost and countries?
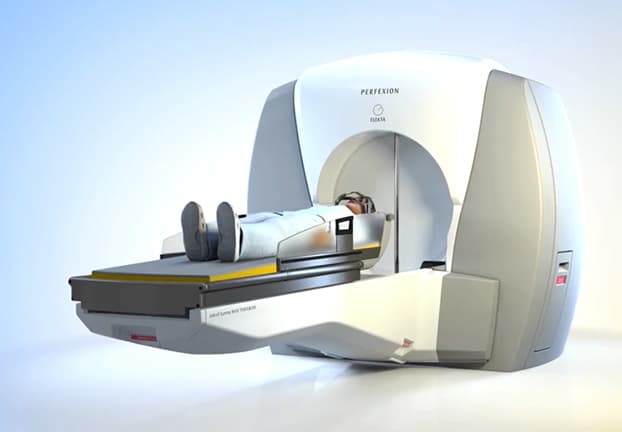
Brain Tumor Treatment Without Surgery in Turkey
Discover more about Gamma Knife surgery in Turkey by reading further. The article covers the procedure itself, expenses involved, and highlights the top clinics and skilled doctors in the country.
Our doctor is highly skilled and an expert in their field.